 Price Vision Group Celebrates 25 Years of LASIK, the first in the state of Indiana.
Price Vision Group Celebrates 25 Years of LASIK, the first in the state of Indiana.
January 2020 marks the 25-year anniversary of Price Vision Group providing LASIK eye surgery. We continue to see happy patients from those early years when Dr. Price performed LASIK as part of an investigational study.
From the start, we were able to correct both nearsightedness and astigmatism. Over time we have continued to refine vision correction options and now provide the most cutting-edge, vision-optimizing treatments available in the U.S.
We began offering refractive surgery in 1983, 37 years ago! We began using a laser to correct vision in 1991. We initially offered surface ablation and in 1995 we began offering LASIK.
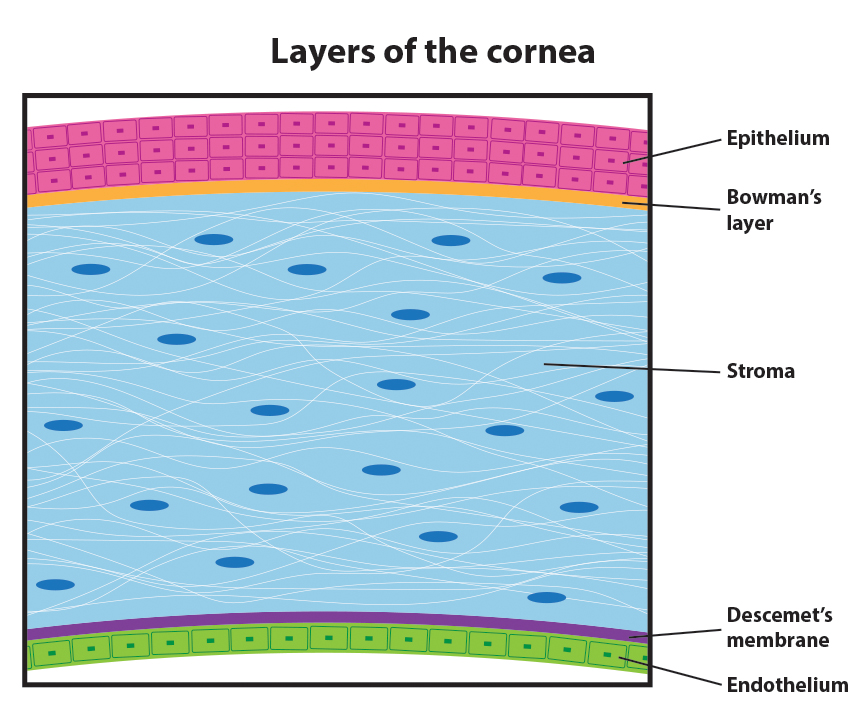
Technological advances in the past 25 years have further improved the safety and accuracy of LASIK. We can now perform topography directed treatments, Contoura™ Vision LASIK, in which we plot 22,000 points on the cornea to generate a topographic map. This allows us to smooth out small imperfections on the corneal surface that cannot be corrected with glasses.
In the clinical trials that led to FDA approval of topography directed treatments, 30% of the patients could see better postoperatively without any correction than they could see preoperatively using glasses.1 Our patients are achieving these same amazing results. In fact, most of our patients achieve better than 20/20 vision.
A vision of 20/20 means that your vision is normal, but surprisingly only 35% of all adults have 20/20 vision without some type of correction, such as glasses. If you have 20/20 vision, you can see at 20 feet what most people see at the same distance. If you are 20/16, you can see at 20 feet what a person with normal vision would need to move up to 16 feet to see, and if you are 20/12, you can see at 20 feet what others would need to move up to 12 feet to see. These are fantastic, life-changing results!
At Price Vision Group, we are proud to be at the forefront in researching the newest in laser vision correction technology. We will soon be investigating whether we can further improve upon LASIK technology with even more sophisticated imaging and analysis. Both the topography-directed treatment and the next-generation treatment rely more on objective imaging of the eye rather than relying so heavily on the subjective assessment of “which is better, 1 or 2”, for greater precision.
As we look back with pride at all that we have accomplished in 25 years, we are also excited about the new technologies we are and will be investigating to provide our patients with the best possible visual outcomes in the safest and most effective ways.






 Pioneering cornea surgeon
Pioneering cornea surgeon 

 Indianapolis, IN – Price Vision Group is pleased to announce its participation in the 2nd annual National Sight Week (October 15-21), sponsored by the American Society of Cataract & Refractive Surgery (ASCRS) Foundation.
Indianapolis, IN – Price Vision Group is pleased to announce its participation in the 2nd annual National Sight Week (October 15-21), sponsored by the American Society of Cataract & Refractive Surgery (ASCRS) Foundation.